22 years old female with previous history of transverse myelitis with acute urinary retention
This is online E log book to discuss our patient’s de-identified health data shared after taking
his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through
series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome."
" I’ve been given this case to solve in an attempt to understand the topic of “patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis and treatment plan "
Unit posting (Intern 2017)
Medical Ward
GM II
Dr Nikitha
Dr Pavan
Dr Lohith
Dr Stimita
CHIEF COMPLAINTS
Patient came to the OPD with chief complaints of acute urinary retention since 11-12
hours (according to her, since last night).
WHAT WE DID OPD BASIS ?
Her history was-
Last night around 12-1 AM she passed urine last time.
Then inspite of feeling bladder fullness, she was unable to pass urine.
And we knew that she had a history of transverse myelitis and she was treated in our
hospital 1 year ago.
On examination, supra pubic bulge was present.
We inserted Foley's catheter in casualty and she voided around 560 ml. and we admitted the patient for further monitoring and evaluation.
HISTORY OF PRESENTING ILLNESS
Patient was apparently asymptomatic till last night(around 12-1am) then she developed acute urinary retention.
Last night around 12-1 AM she passed urine last time.
Then inspite of feeling bladder fullness, she was unable to pass urine.
Events after she got discharged-
▪︎ she gave h/o fever on and off 1-2 episodes a month, low grade, occasionally a/w chills
and rigor, a/w headache.
She uses DOLO 650 mg and fever subsidies on medication.
▪︎h/o tingling sensation in both the lower limbs on and off.no aggravating or relieving factors.
▪︎ h/o headache on and off, usually during fever but sometimes without fever as well.not a/w photophobia,phonophobia,lacrimation.
▪︎ h/o an abortion 6 months ago.(at first trimester)
▪︎ She gets interrupted sleep since few months.
PAST HISTORY :
•N/K/C/O HTN,DM,epilepsy, CVA,CAD,Asthma
•H/o 3 abortions
• surgical history-LSCS 3 years ago
She had a past history of Transverse myelitis. she was admitted,diagnosed and treated in our hospital.
The blog by Dr. Vasistha on this case added here.
MARITAL AND OBSTETRICS HISTORY
Why to stress over this history?
IS THERE ANY CONNECTION BETWEEN HER ILLNESS AND HER ABORTIONS ?
PERSONAL HISTORY :
She is studied till 10th grade, then she got married at the age of 15 years.It was an
arranged marriage and secondary consanguineous marriage.
She has a 7 years of marriage life and a 3 years old daughter.
She does household works, takes care of her daughter as well as farming along with
her husband.As her mother-in-law has knee pain,patient herself has to do all the
household works even when she gets fever episodes,inspite of feeling weak,tired and
lethargic.After getting discharged from our hospital,first few months she was scared
if she gets the same problem again, but now she's not worried about it.
Her daily routine roughly -
She wakes up around 5:30 AM, freshing up,preparing breakfast,lunch for all the
family members(usual South Indian dishes e.g- idli, dosa,sambar,rice).They have their
breakfast around 9 AM then she goes for work along with her husband or does
household work. They usually come back around 1-1:30PM ,eat their lunch.In the
afternoon she takes care or her buffaloes.In the evening she again prepares dinner
(usual South Indian dishes),eats and sleeps around 9 PM.She is non vegetarian.
Since few months, patient has been getting Interrupted sleep.She wakes up 2-3 times in the night.
She doesn't have any addictions.
General examination
Well informed consent is taken. Examined in a well lit room.
Patient is conscious coherent and coperative well oriented to time place and person.
Moderately built and moderately Nourished.
Vitals
Afebrile
BP 110/80mmhg
PR 84bpm
Respiratory rate 15 cpm
There is no icterus, clubbing, cyanosis or lympathadenopathy,Pedal Edema.
Mild pallor was seen.
Systemic examination
Abdominal examination
INSPECTION:
•Shape – scaphoid
Flanks – free
Umbilicus –central in position , inverted.
All quadrants of abdomen are moving equally with respiration.
No dilated veins, hernial orifices, sinuses
No visible pulsations.
PALPATION:
•No local rise of temperature and tenderness
All inspectory findings are confirmed.
No guarding, rigidity
Deep palpation- no organomegaly.
PERCUSSION:
•There is no fluid thrill , shifting dullness.
Percussion over abdomen-
tympanic note heard.
AUSCULTATION:
Bowel sounds are heard.
Cardiovascular system examination
INSPECTION:
•Chest wall - bilaterally symmetrical
No dilated veins, scars, sinuses
PALPATION:
•Apical impulse is felt on the left 5th intercostal space 1cm medial to mid clavicular line.
No parasternal heave, thrills felt
AUSCULTATION:
•S1 and S2 heard , no added thrills and murmurs heard.
Respiratory system examination
INSPECTION:
•Chest is bilaterally symmetrical
Trachea – midline in position.0
Apical Impulse is not appreciated
Chest is moving normally with respiration.
No dilated veins, scars, sinuses.
PALPATION:
•Trachea – midline in position.
Apical impulse is felt on the left 5th intercoastal space.
Chest is moving equally on respiration on both sides
Tactile Vocal fremitus - appreciated
PERCUSSION:
The following areas were percussed on either sides-
Supraclavicular-resonant
Infraclavicular- resonant
Mammary- resonant
Axillary- resonant
Infraaxillary- resonant
Suprascapular- resonant
Infrascapular- resonant
interscapular - resonant.
AUSCULTATION:
•Normal vesicular breath sounds heard
No adventitious sounds
CNS EXAMINATION:
HIGHER MENTAL FUNCTIONS:
Oriented to time place and person
Immediate memory:Intact
Short term memory:Intact
Longterm memory:Intact
No delusions and hallucinations.
CRANIAL NERVES:
NORMAL
-Olfactory nerve(I): Smell is intact
-Optic nerve(II):size of both pupils equal.
Pupil reactivity to light:present
Direct and indirect light reflex are present in both eyes.
-Oculomotor(III),Trochlear(IV)and Abducens(VI):ocular movements present.No
diplopia,No ptosis,No Horizontal Nystagmus
-Trigeminal(V): Sensations over the face present.
Corneal reflex:present
Jaw jerk: present
Muscles of mastication:Normal(No wasting)
-Facial nerve(VII): No deviation of mouth
The wrinkles on both sides of forehead are present.
Taste:intact.
Secretions:Normal in eyes.
-Vestibulocochlear nerve(VIII):Hearing intact.
No positional vertigo and nystagmus.
-Glossipharyngeal (IX) and Vagus(X): uvula is centre and pilatoglossus pillars are
normal and gag reflex intact.
Taste sensations from posterior tongue is normal.
-Spinal accesory(XI):Trapezius and Sternocleidomastoid normal.
-Hypoglossal(XII): Tongue (opening )central in postion.
No weakness and wasting of tongue.
Tongue moments normal.
Neck stiffness:- No
Kernig sign :- No
SENSORY EXAMINATION
Right Left
Spinothalamic
Crude touch + +
Pain + +
Temperature + +
Dorsal column
Fine touch Lost in bilateral soles
Vibration
Olecranon p 6s 5s
Styloid process 7s 10s
Tibia 4s 8s
Medial mallelous 6s 10s
MOTOR EXAMINATION
Tone :- Right. Left
Upper limb. Normal. Normal
Lower limb. Normal. Normal
Power:- Right Left
Upper limb. 5/5. 5/5
Lower limb. 5/5. 5/5
Reflexes :- Right Left
Biceps. + +
Triceps + +
Supinator. - -
Knee. ++ ++
Ankle. ++ ++
Plantar. Flexor Flexor
T11-12 Reflexes absent
Beaver's sign negative
● Lower limb examination in detail, done to localise anatomy of lesion:
Power:- Right Left
HIPS
ILEOPSOAS (L1-L3) 5/5 5/5
ADDUCTOR FEMORIS (L5-S1) 4-/5 4-/5
G MAXIMUS (L5-S1) 4-/5 4-/5
G MEDIUS, MINIMUS (L2-L3) 4-/5 4-/5
THIGH
HAMSTRINGS (L4-S1) 4-/5 4-/5
QUADRICEPS (L3-L4) 4+/5 4+/5
ANKLE
TIBIALIS ANTERIOR (L4-L5) 4-/5 4-/5
TIBIALIS POSTERIOR (L4) 4-/5 4-/5
PERONEI (L5, S1) 4-/5 4-/5
GASTROCNEMIUS (S1) 4-/5 4-/5
FOOT, GREAT TOE
EXT. DIG. LONGUS (L5) 4-/5 4-/5
FL. DIG. LONGUS (S1, S2) 4+/5 4+/5
EXT. HAL. LONGUS (L5, S1) 4-/5 4-/5
EXT. DIG. BREVIS (S1) 4-/5 4-/5
- No finger nose in coordination
- No knee - heel in coordination
INVESTIGATIONS :
Hemogram:
Hb: 9.3 gm%
TLC: 6700
PCV: 29.8
MCV: 71.0
MCH: 22.1
MCHC: 31.2
RBCs: 4.20 millions/cumm
PLT: 3.63 laks/cumm
ECG
USG ABDOMEN AND PELVIS
PROVISIONAL DIAGNOSIS:
LMN Type Neurogenic Bladder
?Recurrent Transverse Myelitis
?Neuromyelitis Optica Spectrum Disorder
TREATMENT:
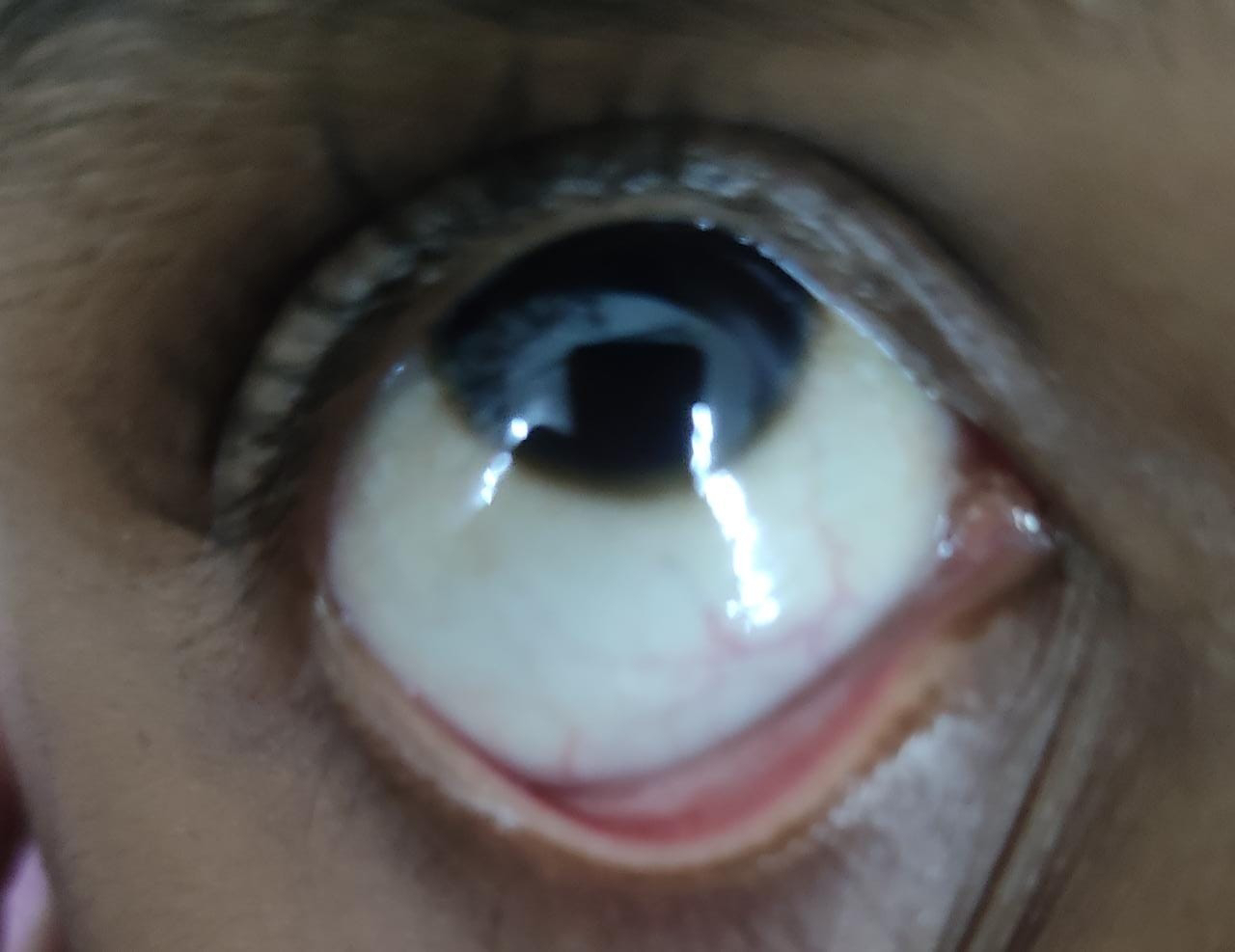
Ophthalmology opinion was taken for this patients.
Impression: Normal fundus study.
Advice:
1.E/d LUBREX 5 times/day
2.Use glasses(Myopic glasses)
Neurology opinion was taken on 29/6/2023
and she adviced-
1.Inj.METHYLPREDNISOLONE 1gm in 100ml of NS once a day for 5 days.
2.Inj.Pantocid 40mg OD/BBF for 5 days at 8 AM
3.Tab.AZORAN 25 mg once daily at 2 PM
4.E/d LUBREX 5 times/day FOR 5 days
PROGRESSION:
We started giving 1gm METHYLPREDNISOLONE in 100 ml of NS under observation, And on the 3rd day she passed urine(Foley's catheter was removed)










Comments
Post a Comment