15 years old school student with chest pain.
This is an E log book to discuss our patient's de-identified health data shared after taking his guardian's signed informed consent. Here we discuss our individual patient problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable comments in comment box are most welcomed
I have been given this case to solve in an attempt to understand the topic of "Patient clinical data analysis" to develop my competency I reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
Long case
Stimita Maity
H.tno 1701006178
Chief complaints
A 15 years old male presented with the complaints of chest pain and heaviness in the left side of the chest since 3 months.
History of present illness
Patient was apparently asymptomatic 3 months ago,then he developed pain and heaviness in the left side of the chest.
** Pain was insidious in onset, gradually progressive, squeezing type,non radiating, aggravated on exercise and relieved on taking rest.
For chest pain he was given Pantoprazole for 10 days but didn't get subsided.
** Heaviness in the chest increased on lying on the left side.
** h/o evening rise of temperature ( around 4:30)
** h/o easy fatiguability
** No h/o cough, haemoptysis, breathlessness, wheezing
Past history
** 4 years ago he developed generalised body and joint pain and was managed in a govt hospital by paracetamol.
** 2 years ago he developed pain in the left side of face and was diagnosed with herpes managed medically
** not a known case of Hypertension, diabetes,epilepsy, TB,Asthma
** no h/o any direct trauma or surgery in the chest
Birth history
Normal vaginal delivery at term
Cried soon after birth
No TORCH infection after birth or in mother during pregnancy
Colostrum fed
He was breastfed only for 1 month as he developed chronic diarrhoea at the age of 9 days so local doctor said to stop breastfeeding and also was managed by some injection.
So from the age of 1 month he was fed outside milk,barley.
Immunized.
Personal history
Takes mixed diet( does not eat vegetables ,consumes less water)
Gets adequate sleep
Appetite normal
Bladder movement regular
H/o constipation
No addiction
H/o dust allergy
Family history
No h/o Tb in family members
Grand father and grandmother have asthma
Mother has dust allergy
Treatment history
Treatment for chronic diarrhoea at 1 month of age
Treatment for generalised body pain 4 yrs ago
Treatment herpes 2 yrs ago
Examination
General examination
Well informed consent was taken. Patient was examined in a well lit room.
Patient was conscious, coherent and cooperative, well oriented to time,place and person. Moderately built and moderately Nourished.
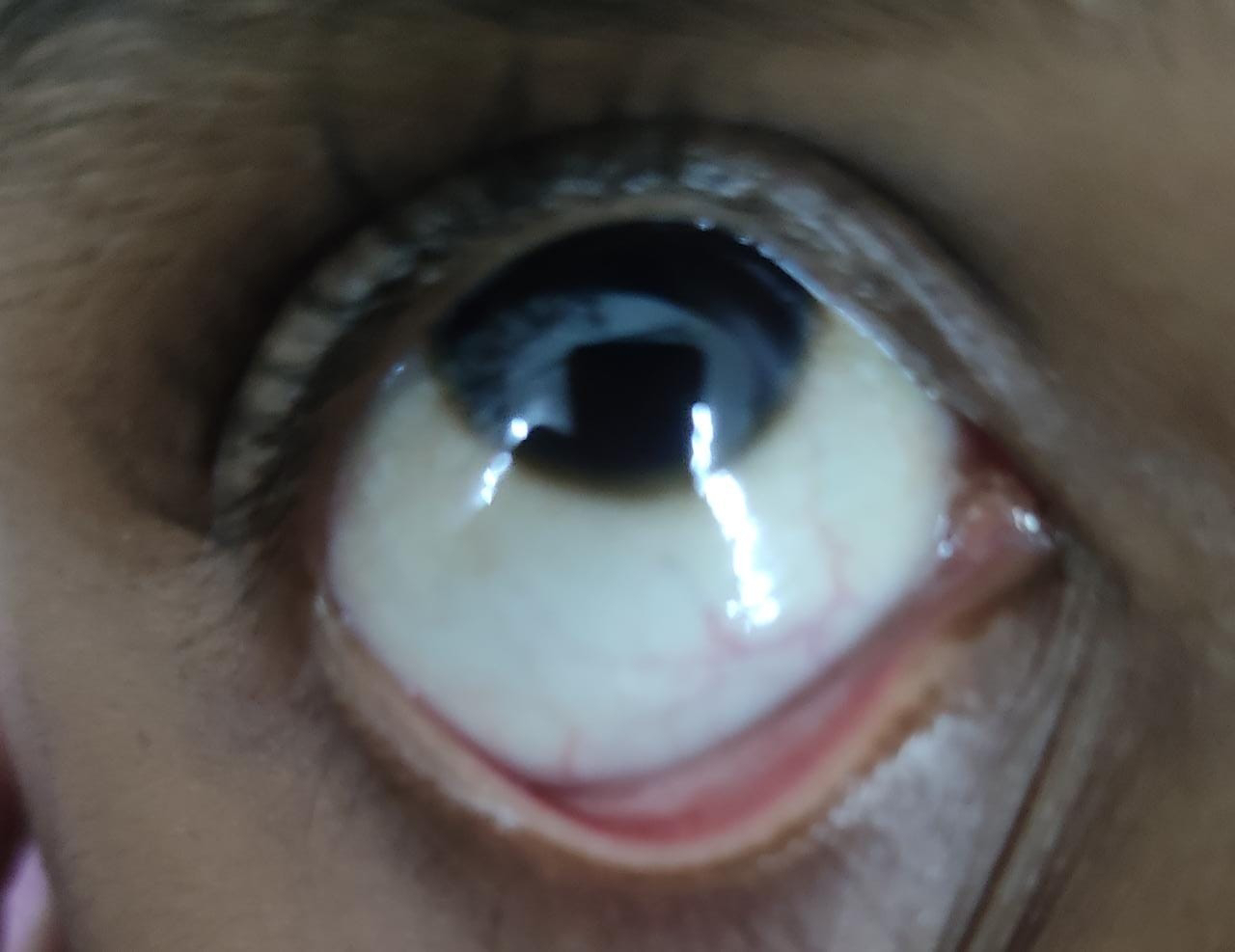
There is no pallor,icterus,clubbing, cyanosis,pedal edema lympathadenopathy.
Vitals
Afebrile
BP 110/70 mm of hg
PR 72bpm
RR 18cpm
Respiratory system examination
Inspection
examination of oral cavity : normal
Nose normal
Shape of chest elliptical
Expansion of chest symmetrical
Trachea: central in position
Apical impulses : not visualised
no drooping shoulder
No crowding of ribs
No supra or infraclavicular fullness or hollowness
No sinus,scar
No kyphoscoliosis
Palpation
Inspectory findings are confirmed.
Trachea : central
No local rise of temperature
No tenderness
Expansion of chest symmetrical
Tactile vocal fremitus : felt,decreased on left side in infraaxillary and infrascapular region
Apex beat at 5th intercostal space medial to midclavicular line.
Percussion
Direct on clavicle : resonant
Supraclavicular,infraclavicular,mammary,inframammary,suprascapular,interscapular,axillary : resonant
Infraaxillary and infrascapular : dull note
Shifting dullness present
Auscultation
Bilateral air entry present
vesicular breath sound heard
Decreased intensity of breath sound at left infraaxillary and infrascapular area.
No added sound
Respiratory system examination
Chest expansion
Abdominal examination
INSPECTION:
•Shape – scaphoid
Flanks – free
Umbilicus –central in position , inverted.
All quadrants of abdomen are moving equally with respiration.
No dilated veins, hernial orifices, sinuses
No visible pulsations.
PALPATION:
•No local rise of temperature and tenderness
All inspectory findings are confirmed.
No guarding, rigidity
Deep palpation- no organomegaly.
PERCUSSION:
•There is no fluid thrill , shifting dullness.
Percussion over abdomen-
tympanic note heard.
AUSCULTATION:
Bowel sounds are heard.
Cardiovascular system examination
INSPECTION:
Chest wall - bilaterally symmetrical
No dilated veins, scars, sinuses
PALPATION:
•Apical impulse is felt on the left 5th intercostal space 1cm medial to mid clavicular line.
No parasternal heave, thrills felt
AUSCULTATION:
•S1 and S2 heard , no added thrills and murmurs heard.
Central nervous system examination
CENTRAL NERVOUS SYSTEM EXAMINATION.
HIGHER MENTAL FUNCTIONS:
•Patient is Conscious, well oriented to time, place and person.
All cranial nerves - intact
Motor system: Intact
Superficial reflexes and deep reflexes are present , normal
Gait is normal
No involuntary movements
•Sensory system -
-All sensations pain, touch,temperature, position, vibration, are well appreciated.
Investigations
CBP : HB 13.2gm%
Tc 6300
N 52%
L 37%
E 2%
M 9%
B 0
Serology negative
Chest x ray
CT scan
Bacterial culture
Bronchoscopy
USG
Left sided hydropneumothorax
Treatment
Treatment
O2 inhalation with nasal prongs with 2 ltrs /mint
Nebulization with duolin
Tab dolo 650mg sos
Advice at discharge:: paracetamol If temp above 99F
Avoid strenuous exercise











Comments
Post a Comment