35 years old male with noisy breathing
35 years old male with noisy breathing
This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through
series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome."
" I’ve been given this case to solve in an attempt to understand the topic of “patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis and treatment plan "
Unit posting (Intern 2017)
Medical Ward
GM II
Dr Nikitha
Dr Pavan
Dr Lohith
Dr Stimita
CHIEF COMPLAINTS
Patient came with chief complaints of noisy breathing (mainly during sleep) since 7 months.
HISTORY OF PRESENTING ILLNESS
Patient was completely fine 7 months ago then he developed dry hacking cough
and noisy breathing.Noisy breathing is continuously present since 7 months and
more in the night.He wakes up in between his sleep because of cough.Patient says
that his wife also can hear the sound when he sleeps.Noisy breathing is insidious in
onset and gradually progressive.
Not associated with evening rise of temperature,joint pain,hemoptysis.
Cough is non productive, aggravates on supine position,exertion and in the summer
season and relieving factor is sleeping lateral position.
He consulted local physician and took antibiotic for 1 week but wasn't relieve.
Then he consulted another physician and took antibiotic for another 1 week but did not see any result.
Patient gave a c/o left sided chest pain on and off which is non radiating(mostly due to prolonged cough)
PAST HISTORY
No similar complaints in the past.
K/c/o HTN since 2 years and on regular medication.
N/k/c/o DM,epilepsy,TB,Asthma,CAD,CVA
No past surgical history
PERSONAL HISTORY
patient has travel agency business.
Takes mixed diet.
Sleep is interrupted due to cough.
Bowel and bladder movements are regular.
Occasional drinker, drinks 90ml of hard liquor 1-2 times every 3-4 months.
Smokes 1-2 cigarettes/ month. He says that his smoking doesn't aggravates his cough and
He has been chewing 1 packet of ghutka a day for the past 5 years.
No known allergies.
Daily routine:
Patient has a travel agency business and his office is near to his home.
He has a small happy joint family with his wife, child, mother and two sisters.
He wakes up around 7:50 -8 am and has a cup of tea and leaves to work at 9.He takes his
breakfast (his first meal) at 11am. He resumes work till 3pm and he goes back
home,takes bath and takes his meal at home,containing rice,dal,curries,fish etc.Then
he goes back to work at around 5pm and stays there until 10pm. He takes his dinner
between 11pm and 12am and sleeps around 1 am.He lives a sedentary lifestyle,no
physical activities.
His wife and sister say that,he follows a very irregular lifestyle.he wakes up right
before leaving to work, sometimes at 8,just takes a cup of tea and leaves to work
and directly come back to home around 3 pm and takes his lunch.His sister says
about his habit of chewing ghutka and sometimes he takes bath in the night and
doesn't follow any routine bound life.
Family History
No similar complaints in his family.
His father was diagnosed with tuberculosis 5 years ago and took treatment and was
treatment success was confirmed. His father passed away due to complications of
covid infection in 2020. He was a k/c/o diabetes.
General examination
Well informed consent is taken. Examined in a well lit room.
Patient is conscious coherent and coperative well oriented to time place and person.
Moderately built and moderately Nourished.
Vitals
Afebrile
BP 110/80mmhg
PR 84bpm
Respiratory rate 18 cpm
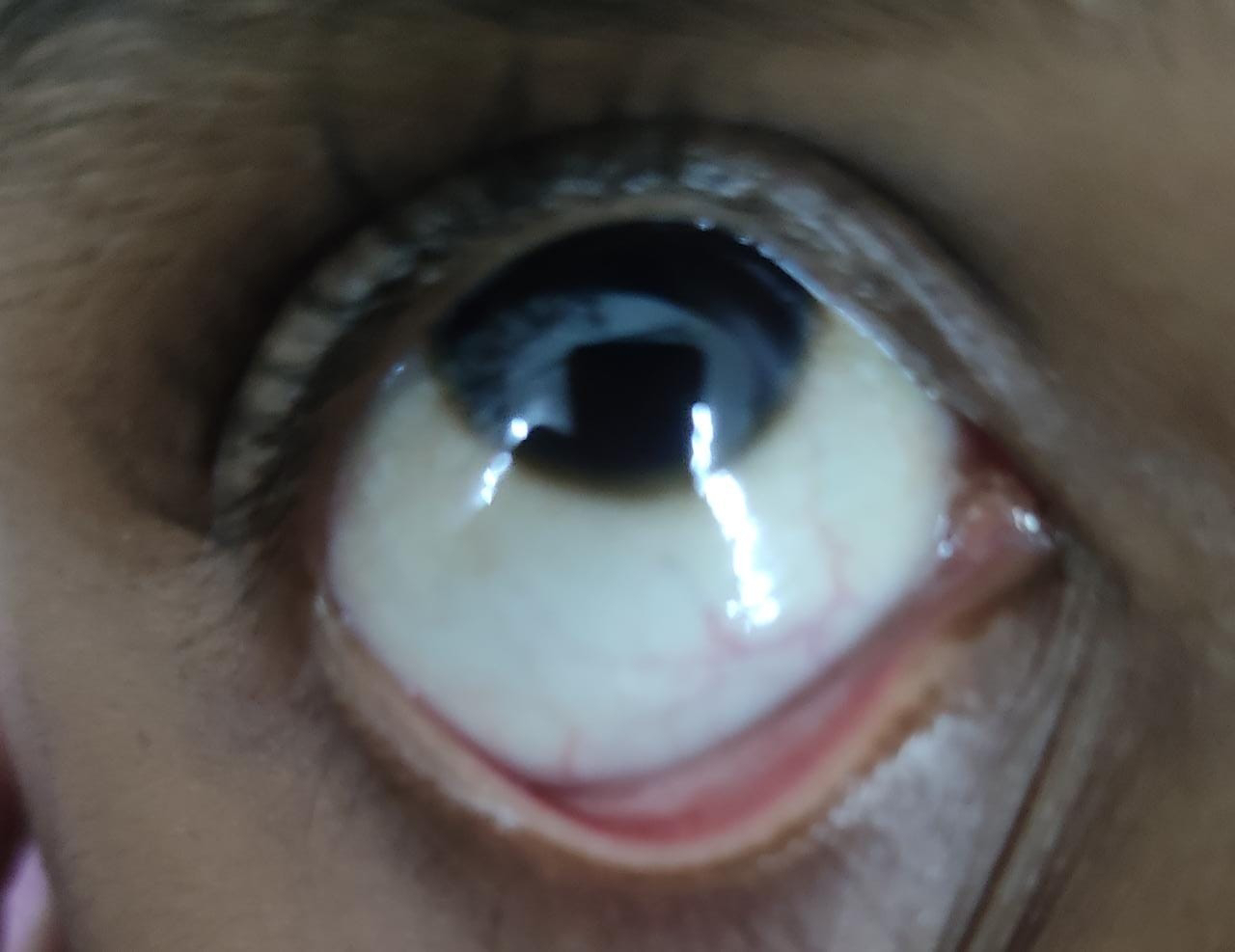
There is no icterus, clubbing, cyanosis or lympathadenopathy,Pedal Edema
Systemic examination
Respiratory system examination
INSPECTION:
•Chest is bilaterally symmetrical
Trachea – midline in position.0
Apical Impulse is not appreciated
Chest is moving normally with respiration.
No dilated veins, scars, sinuses.
PALPATION:
•Trachea – midline in position.
Apical impulse is felt on the left 5th intercoastal space.
Chest is moving equally on respiration on both sides
Tactile Vocal fremitus - appreciated
PERCUSSION:
The following areas were percussed on either sides-
Supraclavicular-resonant
Infraclavicular- resonant
Mammary- resonant
Axillary- resonant
Infraaxillary- resonant
Suprascapular- resonant
Infrascapular- resonant
interscapular - resonant.
AUSCULTATION:
•Normal vesicular breath sounds heard.
Wheeze heard in all the areas.(mainly during expiration)
Abdominal examination
INSPECTION:
•Shape – scaphoid
Flanks – free
Umbilicus –central in position , inverted.
All quadrants of abdomen are moving equally with respiration.
No dilated veins, hernial orifices, sinuses
No visible pulsations.
PALPATION:
•No local rise of temperature and tenderness
All inspectory findings are confirmed.
No guarding, rigidity
Deep palpation- no organomegaly.
PERCUSSION:
•There is no fluid thrill , shifting dullness.
Percussion over abdomen-
tympanic note heard.
AUSCULTATION:
Bowel sounds are heard.
Cardiovascular system examination
INSPECTION:
•Chest wall - bilaterally symmetrical
No dilated veins, scars, sinuses
PALPATION:
•Apical impulse is felt on the left 5th intercostal space 1cm medial to mid clavicular line.
No parasternal heave, thrills felt
AUSCULTATION:
•S1 and S2 heard , no added thrills and murmurs heard.
CNS examination
No abnormality detected
Investigations
Patient has not consented to any investigations as of now.
Provisional diagnosis
Episodic paroxysmal cough in a known case of
hypertension? Asthma?
Treatment:
TAB CETIRIZINE 10mg PO OD
TAB PANTOPRAZOLE 40mg PO OD before breakfast
TAB ULTRACET PO 1/2 QID









Comments
Post a Comment