37 year male with SOB, decreased urine output, abdominal distension
37 year male with SOB, decreased urine output, abdominal distension and facial puffiness, pedal edema
This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through
series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome."
" I’ve been given this case to solve in an attempt to understand the topic of “patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis and treatment plan "
Unit posting (Intern 2017)
Medical Ward
GM II
Dr Nikitha
Dr Haripriya
Dr Govardhini
Dr Stimita
CHIEF COMPLAINTS
Patient came with the chief c/o SOB, decreased passage of urine, abdominal
distension,pedal edema,facial puffiness since 1 day (yesterday morning)
HISTORY OF PRESENTING ILLNESS
Patient was apparently asymptomatic 1 day ago, then he developed -
■ SOB -
Since yesterday morning.
It was sudden in onset(he said that,when it started,he was sitting at time) and aggravates on walking,on supine position and decreases when he sleeps in lateral positionposition(both right and left).
Continuous,non progressive.
It is not associated with chest pain.
No h/o cough,sweating, palpitations.
■ Abdominal distension -
Since yesterday, gradually progressive.
■ Decreased urinary output -
He didn't pass urine from yesterday morning to evening.
Then they called RMP doctor.He gave 1 Injection and 2 tablets(details not available)
⬇️
After 1 hour he passed urine.
⬇️
After that abdominal distension decreased a bit.
There is no loin pain,urgency, frequency,burning micturition,dysuria.
■ Pedal edema -
Since 1 day
Pitting type.
Yesterday it was till knee length, today it decreased and till ankle length.
■ H/o decreased sensation, numbness and tingling sensation in the left lower limb since 10 years.
On asking, he gave a history of fever and pus discharge 4 days ago ,describing below
Patient had purulent secretions from the area just below the scrotum (? fistula) and fever 4 days ago.
⬇️
Then he consulted RMP doctor and took AMOXICILLIN, DOMPERIDONE,PARACETAMOL for 3 days.
⬇️
Then his fever and pus secretions was decreased.
⬇️
But after 2 days he developed edema in both upper and lower limbs and facial puffiness.
⬇️
And SOB,abdominal distension and decreased urine output since yesterday morning.
Patient passed flatus on 28/7/23night.
PAST HISTORY
Patient had a similar history of SOB 6 months ago, grade 4.
For that he went to a hospital in Devarkonda.
There doctor said that there is water accumulation in the chest ( ? Hydrothorax) and that will decrease on taking medication
So, he took medication(detials not available)for 1 month and was cured.
H/o epilepsy 15 years ago and not on regular medication.
N/k/c/o TB,asthma,DM,HTN,CVA,CAD
past surgical history -
Patient fell from the bridge 10 years ago and got spinal injury and spinal surgery was done.
After 3-4 years, he had a thorn prick in the right feet, the infection spreaded(according to patient and the attender)in the leg and amputation was done.
FAMILY HISTORY
Not significant
PERSONAL HISTORY
Patient lives with his wife and 2 daughters.
He stays at home and walks around the home and nearby with the help of Walker after his amputation was done7-8 years ago).
Coming to his life history in short,
10 years ago,
He was auto driver and was living a happy family life with his wife and daughter.
Then he had an accident (he fell from the bridge) and got spinal injury and spinal surgery was done in our hospital.
Then,
7-8 years ago,
He had a thorn prick in the right foot and the infection got spreaded in the right leg.So,Amputation was done.
Since then he has been staying at home.
His wife is daily wage worker, she goes to work and his both the daughters go to school (elder one studies in 12th standard and younger one just started her schooling)and patient lives a daily routine bound life at home.
He was completely fine all these years(didn't visit hospital)
But 6 months ago,
He developed SOB,and for that he visited hospital in Devarkonda.
He wakes up around 6 am, after freshing up, takes a cup of tea, spends time at home(eaither sitting,lying on bed or walking around with the help of Walker)
Then he takes his breakfast around 9 am (rice mainly),lunch around 1 pm(rice) and dinner around 8 pm(rice).
He takes mixed diet, appetite is decreased since 4 days.
He was a regular alcoholic but stopped 1 year ago.No other addictions.
No known allergies
GENERAL EXAMINATION
Well informed consent is taken. Examined in a well lit room.
Patient is conscious coherent and coperative well oriented to time place and person.
Moderately built and moderately Nourished.
Vitals
Afebrile
BP 140/80mmhg
PR 60bpm
Respiratory rate 25 cpm
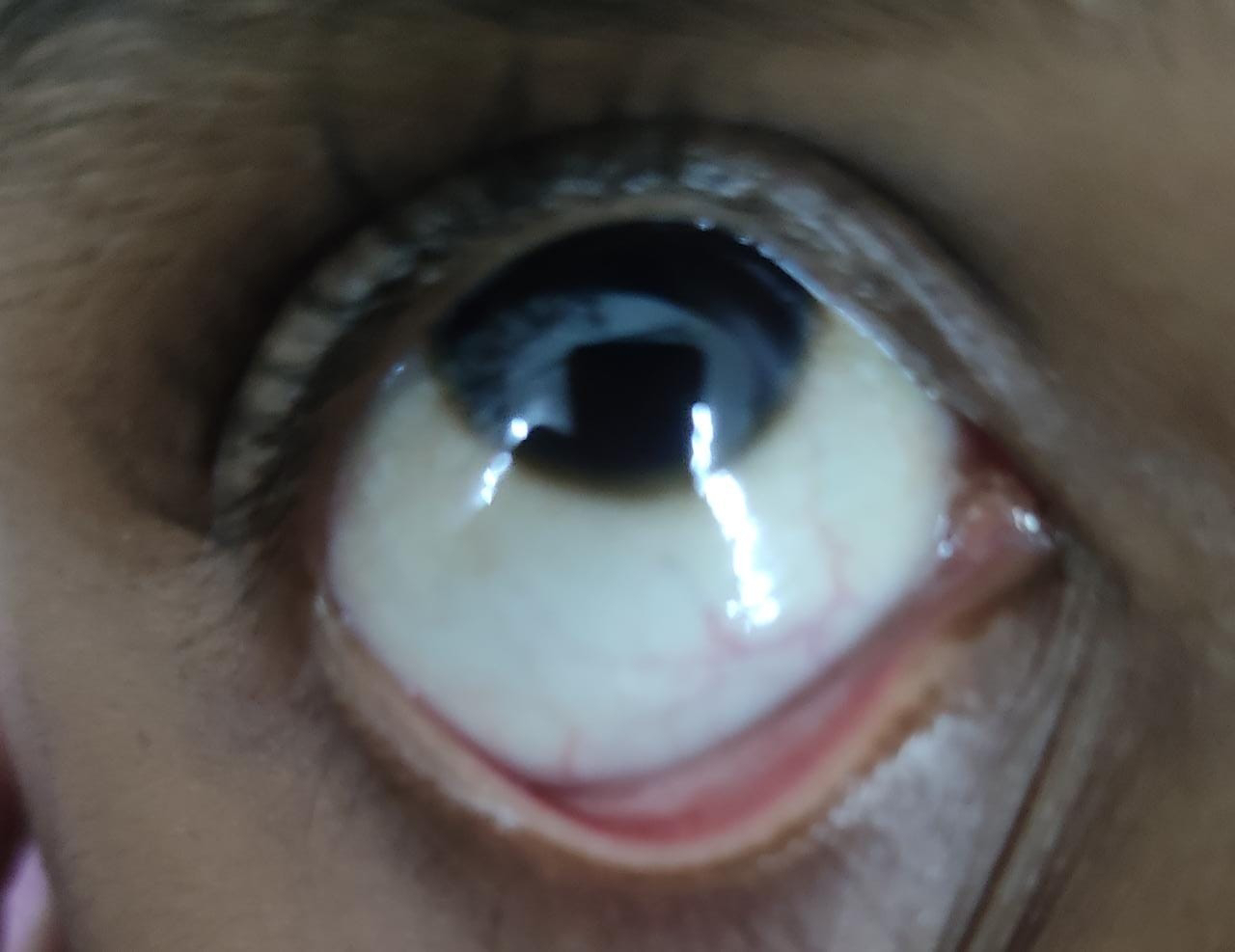
There is no icterus, clubbing, cyanosis or lympathadenopathy.
Pedal edema present.
No raised JVP
Systemic examination
Respiratory system examination
INSPECTION:
•Chest is bilaterally symmetrical
Trachea – midline in position.0
Apical Impulse is not appreciated
Chest is moving normally with respiration.
No dilated veins, scars, sinuses.
PALPATION:
•Trachea – midline in position.
Apical impulse is felt on the left 5th intercoastal space.
Chest is moving equally on respiration on both sides
Tactile Vocal fremitus - appreciated
PERCUSSION:
The following areas were percussed on either sides-
Supraclavicular-resonant
Infraclavicular- resonant
Mammary- resonant
Axillary- resonant
Infraaxillary- resonant
Suprascapular- resonant
Infrascapular- resonant
interscapular - resonant.
AUSCULTATION:
•Normal vesicular breath sounds heard.
• crepts present at right basal region
Abdominal examination
Distended
Abdominal rigidity present.
Tenderness present in epigastric region.
No fluid thrill
No shifting dullness
CVS examination
S1,S2 heard, no murmurs
CNS EXAMINATION
Motor examination
Right Left
Tone
Upper limb N. N
Lower limb N Amputated
Power
Upper limb 5/5 5/5
Lower limb 5/5. Amputation
Reflexes
Biceps ++. ++
Triceps ++. ++
Supinator ++. ++
Knee - Amputation
Ankle -
Plantar -
Loss of fine,crude touch, temperature and proprioception Left lower limb (till ankle)after Spine surgery secondary to trauma 10yrs ago
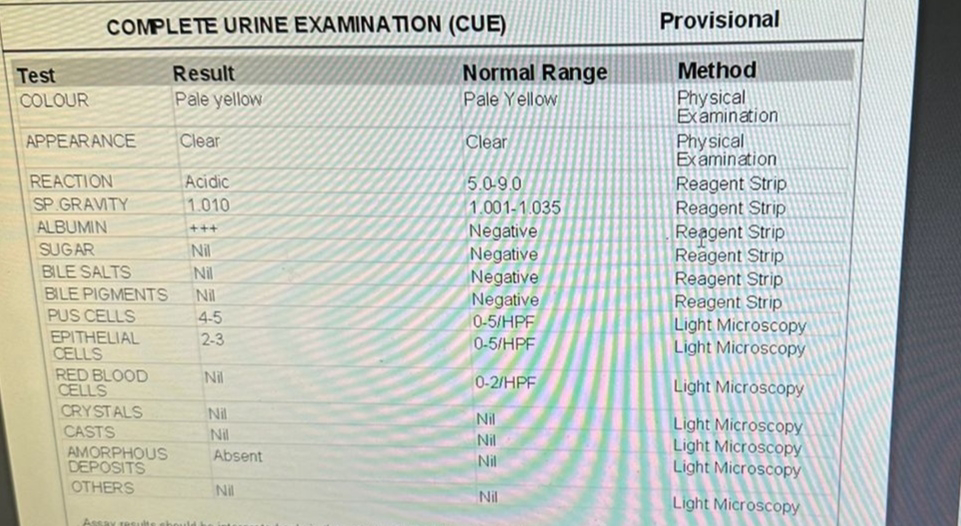
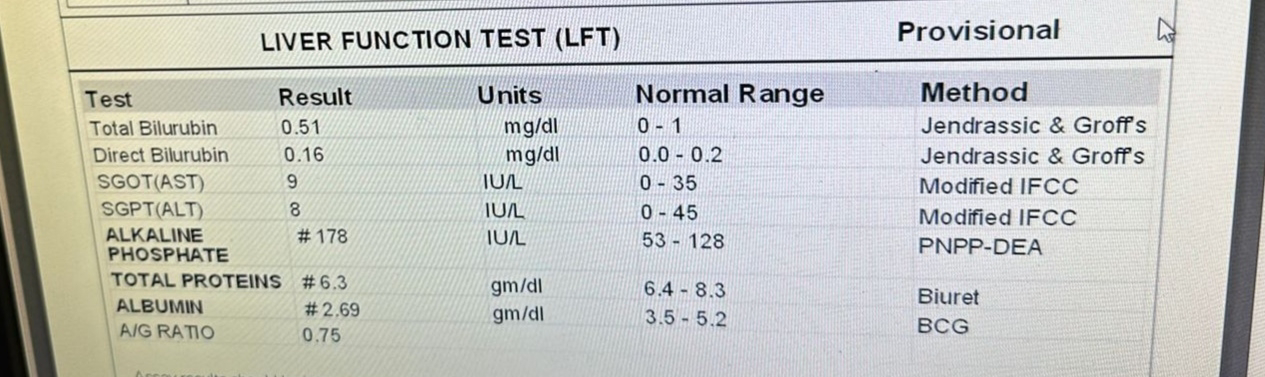
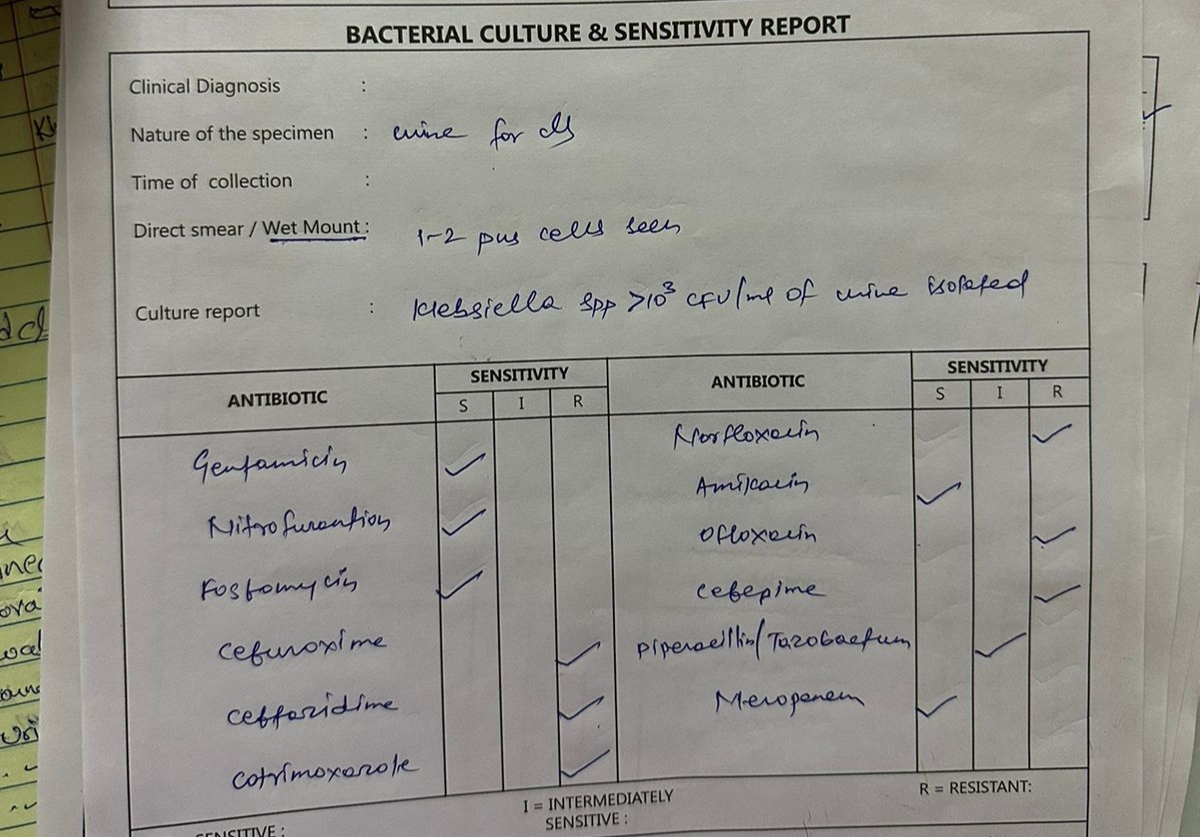
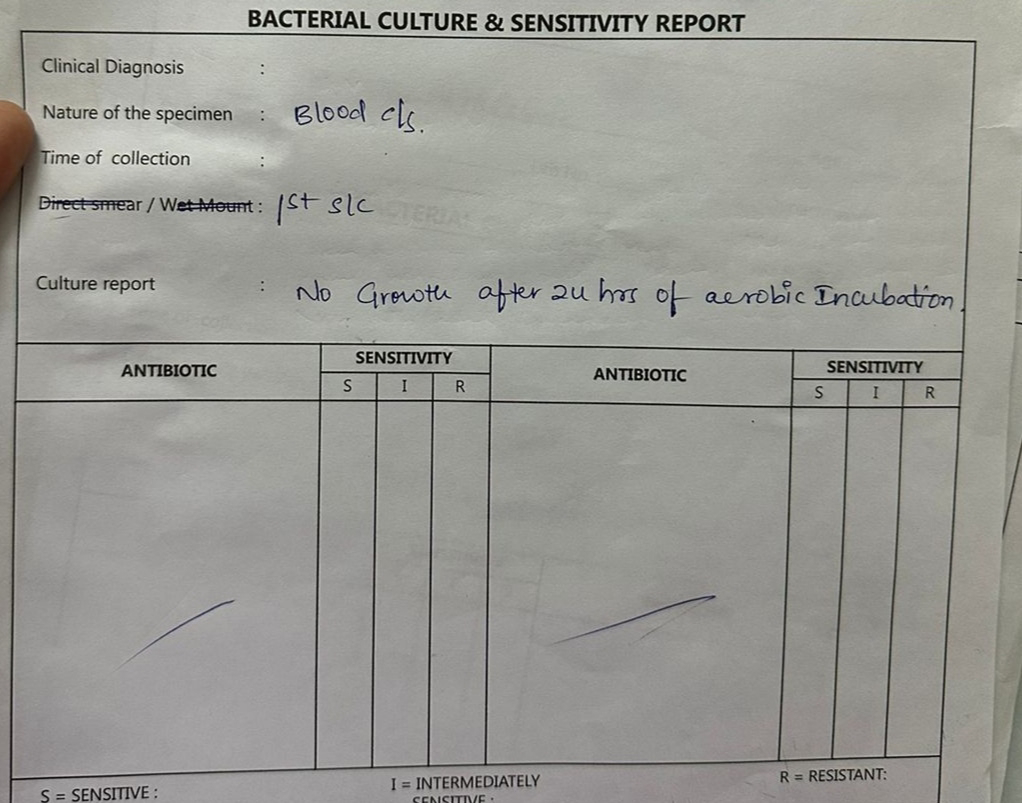
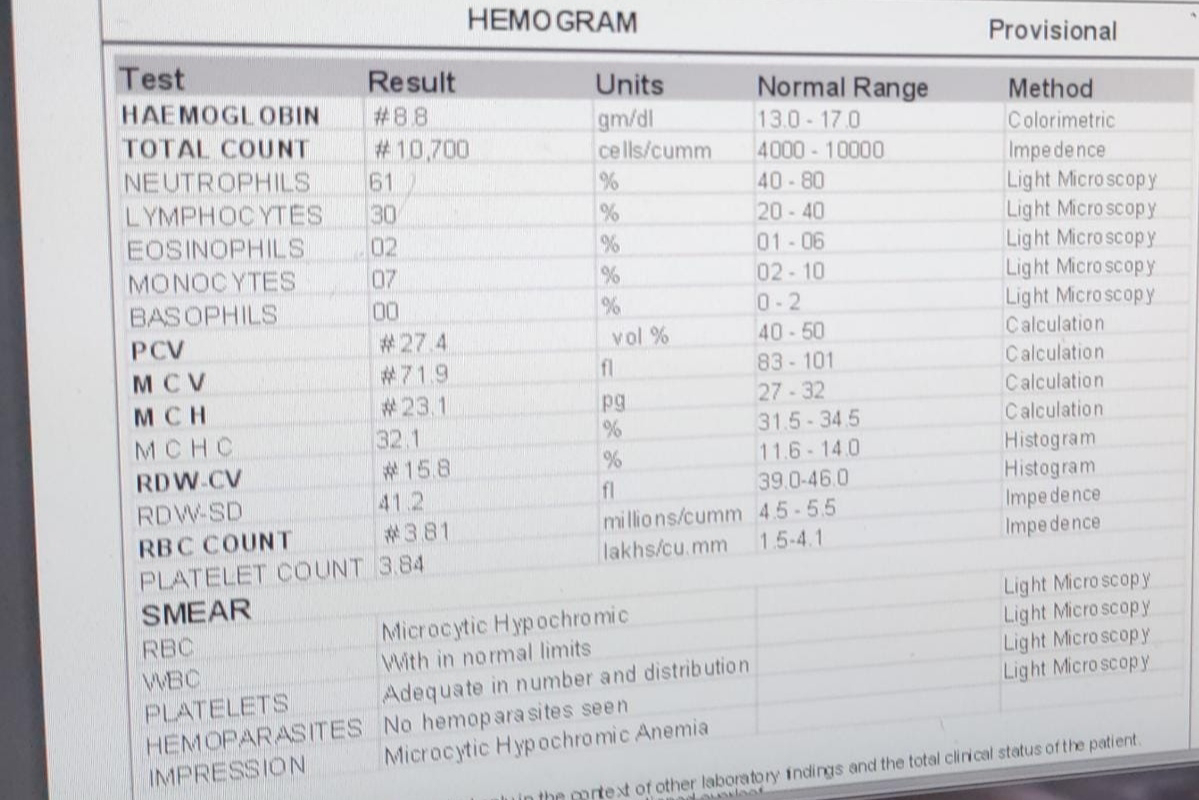
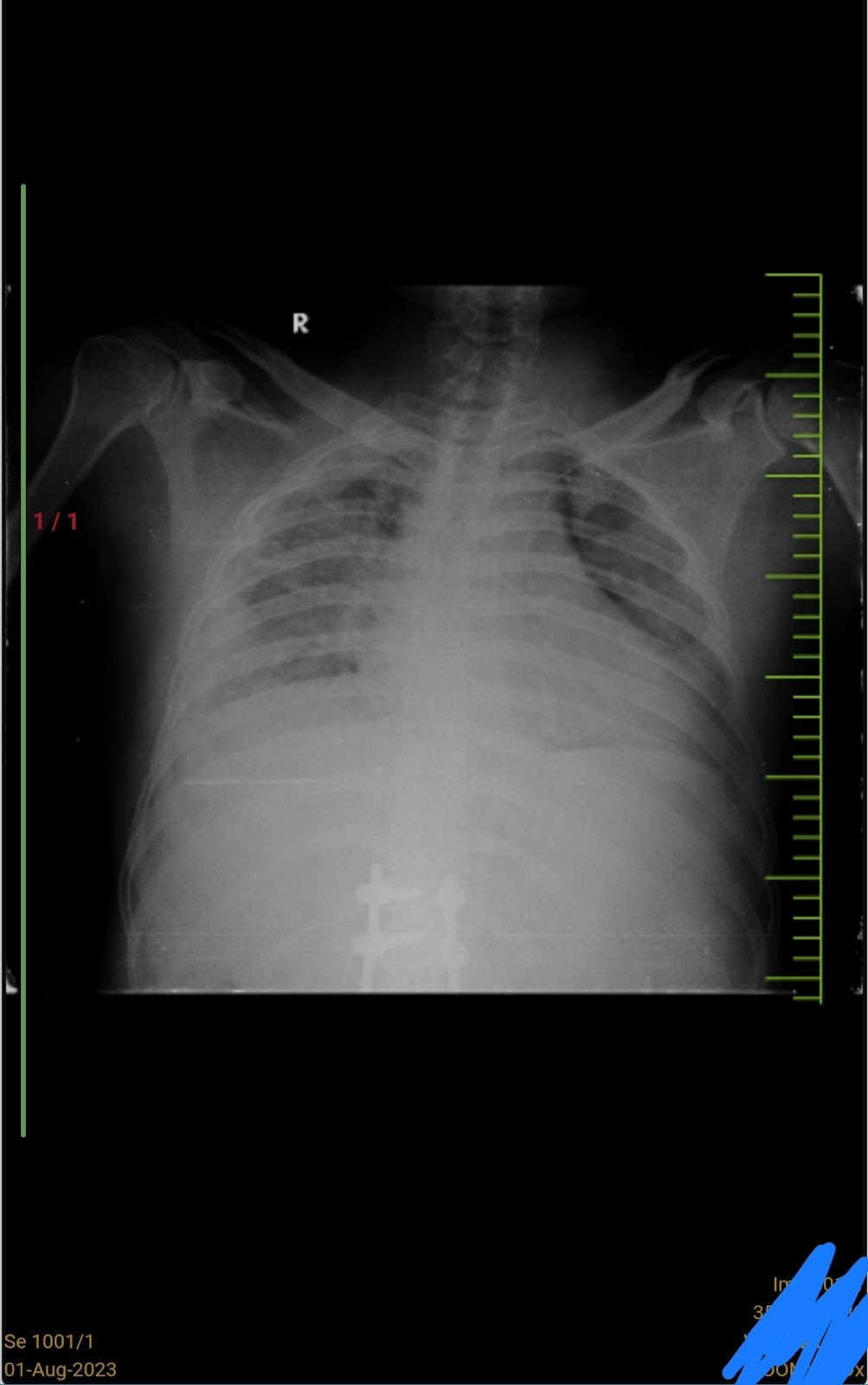
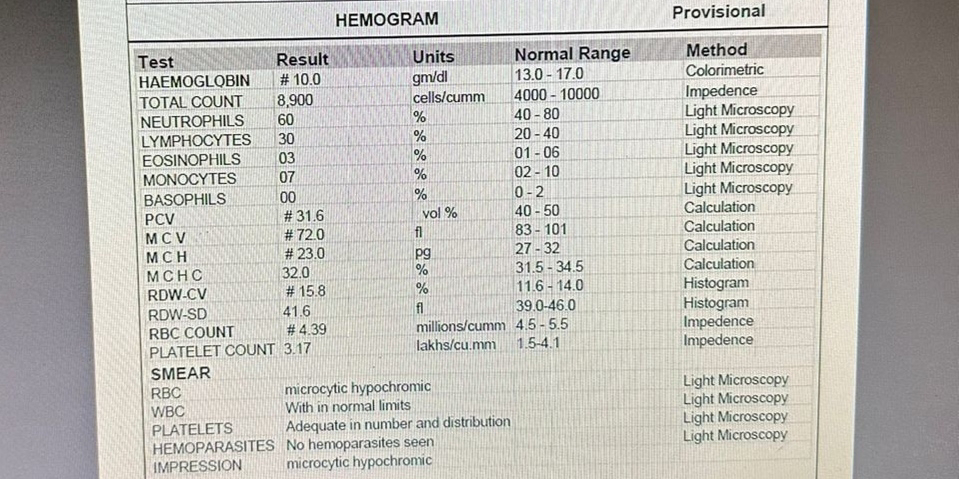
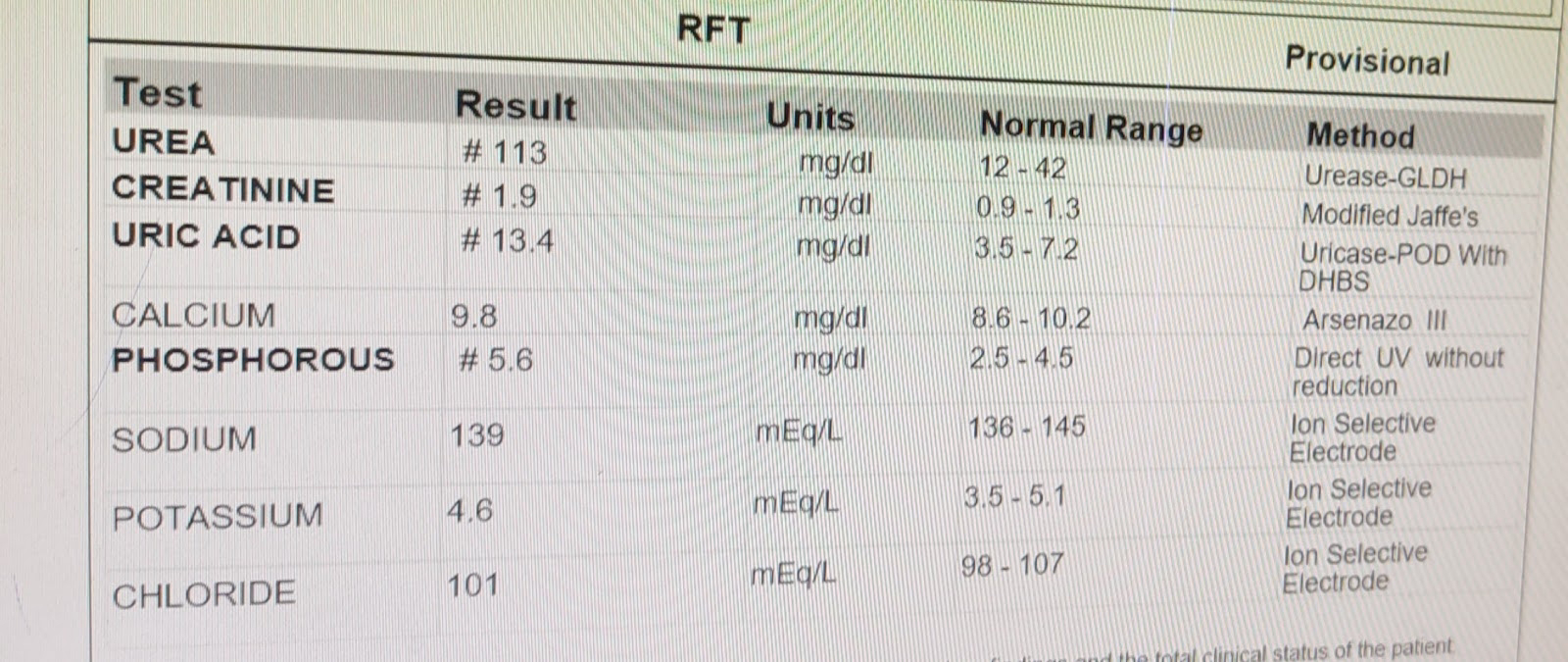
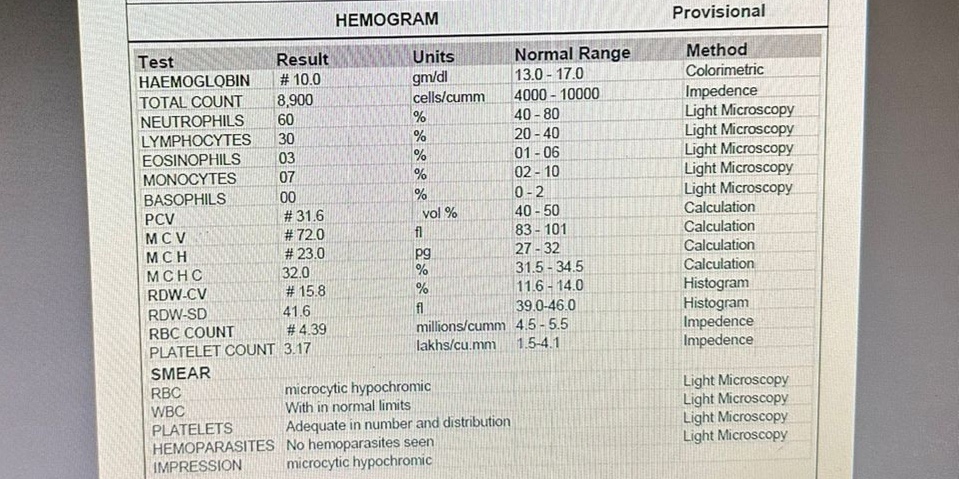
INVESTIGATION
On 28/7/23
ECG ON 28/7/23
Usg on 28/7/23
Ecg on 30/7/23 (12am)
Ecg on 30/7/23(8am)
1/8/23
3/8/23
4/8/23
5/8/23
PROVISIONAL DIAGNOSIS
ANASARCA SECONDARY TO HFpEF WITH MODERATE PAH WITH CKD WITH DENOVO HTN
TREATMENT
1. Inj. Lasix 40 mg IV/BD
2. INJ. PAN 40 mg IV/OV/BBF
3.PROTEIN POWDER 2 SCOOPS IN 100 ML MILK OR WATER
5.TAB. OROFER-XT PO/OD
6.TAB.SHELCAL -CT PO/OD
7.CAP. BIO D3 PO/ONCE A WEEK
Soap notes
30.07.2023
Medicine ward
DR.NIKITHA(SR)
DR.HARI PRIYA(PGY2)
DR.GOVARDHINI(PGY1)
S:
SOB not decreased,
Stool not passed,
Flatus passed
Pedal edema not decreased
Urine output(from yesterday night 9pm to today morning 9:20 am)- 250 ml
O:
Pt is c/c/c
Pallor present
BP - 120/70 mmHg
PR- 64bpm
RR - 25cpm
Temp - 98.7 F
GRBS -148 mg/dl
SpO2 - 98% @RA
CVS - S1 S2 heard
RS - BAE+ , Right sided basal crepts present
P/A - distended and non tender
CNS - no FND
A:
PEDAL EDEMA AND SOB UNDER EVALUATION
? AKI (PRE RENAL)
?HEART FAILURE
P:
1.INJ. LASIX 40 MG IV/BD( IF SBP MORE THAN 110 MM OF HG)
2.PROTEIN POWDER 2 SCOOPS IN 100 ML MILK OR WATER
3.TAB. OROFER-XT PO/OD
4.TAB.SHELCAL -CT PO/OD
Soap notes
1.08.2023
AMC
DR.NIKITHA(SR)
DR.HARI PRIYA(PGY2)
DR.GOVARDHINI(PGY1)
S:
SOB increased,
Anasarca increased,
Stool passed,
No fever spike
O:
Pt is c/c/c
Pallor present
BP - 160/100 mmHg
PR- 58bpm
RR - 24cpm
Temp - 98.7 F
GRBS -123 mg/dl
SpO2 - 98% ON CPAP
CVS - S1 S2 heard,No murmurs
RS - BAE+ , B/L diffuse crepts present
P/A - distended and non tender
CNS - no FND
Input/Output- 800/900ml
A:
ANASARCA SECONDARY TO HFpEF WITH MOD PAH WITH? CKD
P:
1.INJ. LASIX 40 MG IV/TID( IF SBP MORE THAN 110 MM OF HG)
2.INTERMITTENT CPAP
3.PROTEIN POWDER 2 SCOOPS IN 100 ML MILK OR WATER
4.TAB. OROFER-XT PO/OD
5.TAB.SHELCAL -CT PO/OD
Soap notes
2.08.2023
AMC-BED 2
DR.NIKITHA(SR)
DR.HARI PRIYA(PGY2)
DR.GOVARDHINI(PGY1)
S:
SOB decreased,
Anasarca not subsided,
Stool not passed,
Flatus passed
No fever spike
O:
Pt is c/c/c
Pallor present
BP - 160/100 mmHg
PR- 62bpm
RR - 22cpm
Temp - 98.7 F
GRBS -99 mg/dl
SpO2 - 95% ON RA
CVS - S1 S2 heard,No murmurs
RS - BAE+ , B/L fine basal crepts present
P/A - distended and non tender
CNS - no FND
Input/Output- 850/530ml
A:
ANASARCA SECONDARY TO HFpEF WITH MOD PAH WITH? CKD WITH DENOVO HTN WITH CONSTIPATION UNDER EVALUATION
P:
1. IVF NS @UO + 30 ML/ HOUR
2.INJ. LASIX 40 MG IV/TID( IF SBP MORE THAN 110 MM OF HG)
3.INTERMITTENT CPAP
4.PROTEIN POWDER 2 SCOOPS IN 100 ML MILK OR WATER
5.TAB. OROFER-XT PO/OD
6.TAB.SHELCAL -CT PO/OD
7.TAB. NICARDIA 10 MG PO/TID
Soap notes
3.08.2023
AMC-BED 2
DR.NIKITHA(SR)
DR.HARI PRIYA(PGY2)
DR.GOVARDHINI(PGY1)
S:
SOB decreased,
Anasarca not subsided,
Stool passed yesterday
No fever spike
O:
Pt is c/c/c
Pallor present
BP - 130/80 mmHg
PR- 70bpm
RR - 22cpm
Temp - 98.7 F
GRBS -107 mg/dl
SpO2 - 92% ON RA
CVS - S1 S2 heard,No murmurs
RS - BAE+ , B/L fine basal crepts present
P/A - distended and non tender
CNS - no FND
Input/Output- 1500/700ml
Abdominal girth - 109 CM
Wt- 64 kgs
A:
ANASARCA SECONDARY TO HFpEF WITH MODERATE PAH WITH CKD WITH DENOVO HTN
P:
1. IVF NS @UO + 30 ML/ HOUR
2.INJ. LASIX 40 MG IV/TID( IF SBP MORE THAN 110 MM OF HG)
3.INTERMITTENT CPAP
4.PROTEIN POWDER 2 SCOOPS IN 100 ML MILK OR WATER
5.TAB. OROFER-XT PO/OD
6.TAB.SHELCAL -CT PO/OD
7.TAB. NICARDIA 10 MG PO/TID














































Comments
Post a Comment