YOUNG ONSET OF DM WITH UNCONTROLLED SUGARS WITH GENERALIZED WEAKNESS OF BOTH UPPER AND LOWER LIMBS
YOUNG ONSET OF DM WITH UNCONTROLLED SUGARS WITH GENERALIZED WEAKNESS OF BOTH UPPER AND LOWER LIMBS
This is online E log book to discuss our patient’s de-identified health data shared after taking
his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through
series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome."
" I’ve been given this case to solve in an attempt to understand the topic of “patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis and treatment plan "
Unit posting (Intern 2017)
Medical Ward
GM II
Dr Nikitha
Dr Pavan
Dr Lohith
Dr Stimita
Chief complaints
25 years old male patient came to OPD with a complaint of generalised
weakness of upper and lower limb since 2-3 months.
HOPI
patient was apparently asymptomatic 3 months ago,then he developed
polyuria, nocturia and generalised weakness and visited local hospital and after
getting all Investigations done,he was diagnosed with type 2 diabetes mellitus and
on regular medication (medication not known)
H/o ployphagia, polydypsia.
No h/o burning micturition.
H/o tingling sensation of feet since 2-3 months(no numbness)
H/o headache on and off ,diffuse, throbbing type and relieves on taking medication.
No h/o photophobia, phonophobia.
History of neck pain on and off
H/o SOB on lying down after having food and relieves on sitting position since 3 months.
H/o weight loss (2-3 kgs in 3 months)
Past history
No history of Hypertension, Bronchial Asthma, Epilepsy, thyroid
,tuberculosis ,CVA,CAD
Family history
His father is diabetic since 5 years.
Personal history
He is 25 years old and driver by occupation.He stays with his parents.His basically
leads a sedentary lifestyle because of his occupation, and there is no physical
exercise in his daily routine. He wakes up in the morning around 7-7:30 am then
takes his breakfast(usual south Indian breakfast e.g idli,vada)and goes for his
occupation.He takes his lunch when he gets time(between 1-3 pm), lunch and dinner
also are usual south Indian dishes(rice,dal,sambar). When I kept on asking , he
mentioned that he eats less vegetables and likes to eat more chicken, mutton, fish,
oily spicy fatty food(fast food) and never thought of controlling junk food.He doesn't
smoke but occasionally drinks with friends.
But now when we explained about his health condition,consequences of continuing
his diet pattern and sedentary lifestyle, he said that he will change his diet and
lifestyle.
In short,
He takes mixed diet
Appetite normal
Bowel and bladder movements are regular
Non smoker
Occasional alcoholic
No known allergies
General examination
Well informed consent is taken. Examined in a well lit room.
Patient is conscious coherent and coperative well oriented to time place and person.
Moderately built and moderately Nourished.
Vitals
Afebrile
BP 110/80mmhg
PR 84bpm
Respiratory rate 18 cpm
There is no icterus, clubbing, cyanosis or lympathadenopathy,Pedal Edema

Systemic examination
Abdominal examination
INSPECTION:
•Shape – scaphoid
Flanks – free
Umbilicus –central in position , inverted.
All quadrants of abdomen are moving equally with respiration.
No dilated veins, hernial orifices, sinuses
No visible pulsations.
PALPATION:
•No local rise of temperature and tenderness
All inspectory findings are confirmed.
No guarding, rigidity
Deep palpation- no organomegaly.
PERCUSSION:
•There is no fluid thrill , shifting dullness.
Percussion over abdomen-
tympanic note heard.
AUSCULTATION:
Bowel sounds are heard.
Cardiovascular system examination
INSPECTION:
•Chest wall - bilaterally symmetrical
No dilated veins, scars, sinuses
PALPATION:
•Apical impulse is felt on the left 5th intercostal space 1cm medial to mid clavicular line.
No parasternal heave, thrills felt
AUSCULTATION:
•S1 and S2 heard , no added thrills and murmurs heard.
Respiratory system examination
INSPECTION:
•Chest is bilaterally symmetrical
Trachea – midline in position.0
Apical Impulse is not appreciated
Chest is moving normally with respiration.
No dilated veins, scars, sinuses.
PALPATION:
•Trachea – midline in position.
Apical impulse is felt on the left 5th intercoastal space.
Chest is moving equally on respiration on both sides
Tactile Vocal fremitus - appreciated
PERCUSSION:
The following areas were percussed on either sides-
Supraclavicular-resonant
Infraclavicular- resonant
Mammary- resonant
Axillary- resonant
Infraaxillary- resonant
Suprascapular- resonant
Infrascapular- resonant
interscapular - resonant.
AUSCULTATION:
•Normal vesicular breath sounds heard
No adventitious sounds
CNS EXAMINATION:
HIGHER MENTAL FUNCTIONS:
Oriented to time place and person
Immediate memory:Intact
Short term memory:Intact
Longterm memory:Intact
No delusions and hallucinations.
CRANIAL NERVES:
-Olfactory nerve(I): Smell is intact
-Optic nerve(II):size of both pupils equal.
Pupil reactivity to light:present
Direct and indirect light reflex are present in both eyes.
-Oculomotor(III),Trochlear(IV)and Abducens(VI):ocular movements present.No
diplopia,No ptosis,No Horizontal Nystagmus
-Trigeminal(V): Sensations over the face present.
Corneal reflex:present
Jaw jerk: present
Muscles of mastication:Normal(No wasting)
-Facial nerve(VII): No deviation of mouth
The wrinkles on both sides of forehead are present.
Taste:intact.
Secretions:Normal in eyes.
-Vestibulocochlear nerve(VIII):Hearing intact.
No positional vertigo and nystagmus.
-Glossipharyngeal (IX) and Vagus(X): uvula is centre and pilatoglossus pillars are
normal and gag reflex intact.
Taste sensations from posterior tongue is normal.
-Spinal accesory(XI):Trapezius and Sternocleidomastoid normal.
-Hypoglossal(XII): Tongue (opening )central in postion.
No weakness and wasting of tongue.
Tongue moments normal.
MOTOR SYSTEM:
No visible muscle wasting is seen on inspection.
TONE OF THE MUSCLE:
Right: upper limb—Normal tone
lower limb—Normal tone
Left:Upper limb—-Normal tone
lower limb—-Norma tone.
POWER OF MUSCLE:
Right upper limb: 5/5
(Tested for supraspinatus,Deltoid,infraspinatus,Rhomboid,pectoralis major,latissimus dorsi,biceps, brachioradialus, triceps,Extensor carpi radialis, Extensor carpi ulnaris,Extensor digitorum,Flexor carpi radialis and Flexor carpi ulnaris,Abductor pollicis longus, Extensor pollicis brevis,Extensor pollicis longus,Lumbricals,Abductor digiti minimi.)
Right lower limb:5/5
(Tested for Quadriceps femoris,Tibialis anterior,Tibialis posterior,Gastrocnemius,peronei,Extensor digitorum longus,flexor digitorum longus,extensor digitorum brevis,extensor hallucis longus)
Left upper limb:5/5
Left lower limb:5/5
POSTURE AND GAIT:
No abnormal seen.
No involuntary movements or tremors are seen.
Reflexes Right Left
Biceps. Absent. Absent
Triceps ++ ++
Supinator. ++. ++
Knee. ++. ++
Ankle. ++. ++
Plantar. Mute. Mute
SENSORY SYSTEM:
Spinothalamic
1. Crude touch-present
2.pain-present
3.temperature -present
Posterior column
1.fine touch-+
2.vibration
Olecranon process -N
Styloid process-N
Shaft of tibia-N
Medical malleolus
Cortical
1.graphethesia-+
2.stereognosis-+
3.tactile stimulation -+
Cerebellar function tests:
No ataxia
No dysarthria,tremors,hypotonia
Coordination tests:
Finger nose test: done by both hands(normal).
No overshooting.
Finger to finger testing:no incordination.
Diadokokinesia: normal
Heel knee test: no incordination
Steriognosis : intact
Autonomic nervous system:
No increased sweatin
No postural hypotension
Meningeal signs:
No neck pain
No spinal and cranial abnormalities
No carotid bruit
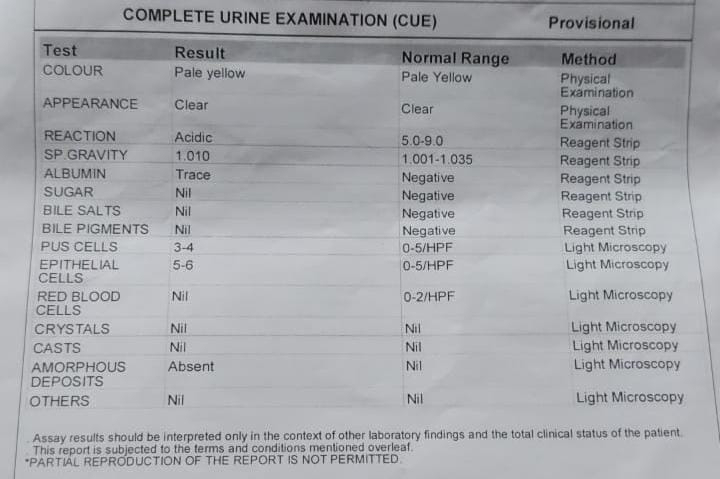
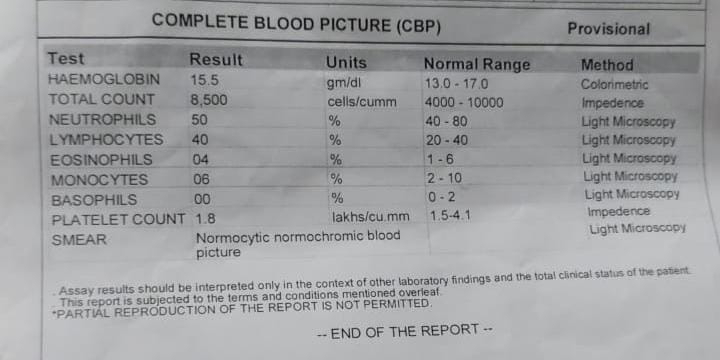
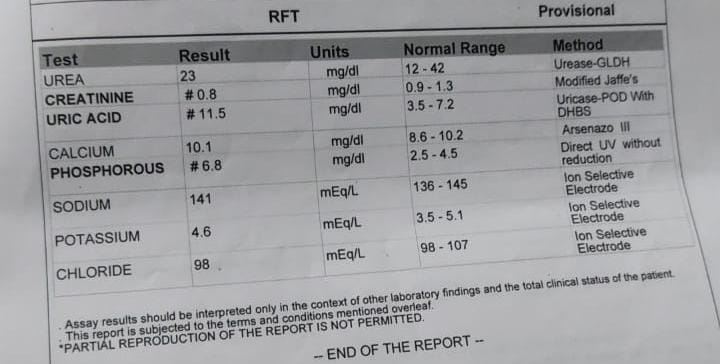
INVESTIGATION
FBS(12/6/23)
DIAGNOSIS
uncontrolled sugars with young onset of diabetes under evaluation with hypertryglyceridemia with hyperbiliribinemia
TREATMENT
1. Inj. HAI according to GRBS SC/TID (PRE MEAL)
2.Inj. NPH SC/BD
3. Tab. FENOFIBRATE 160 mg PO/OD
We started this Treatment in our hospital after admission and 7 point grabs profiles were observed.
So we took Endocrinology opinion on 16/6/23
And he was advised to take
1. Strict diabetic diet
2.15 units of regular insulin s/c premeal(5units -5 units -5 units) and
15 units of NPH(8units- × -7units) everyday
Total 30 units of insulin everyday.
3. And was advised to get one USG abdomen done for his hypertriglyceridemia (which may lead to pancreatitis)-pancreas was normal in size and echotexture
And for his hypertriglyceridemia ,
Gastroenterology opinion was taken on 16/6/23.
Our Gastroenterologist suspected mild hepatitis (but his serology reports were negative)
and he was advised to take
1.Tab. BILYPSA 4mg (saroglitazar) once a day.
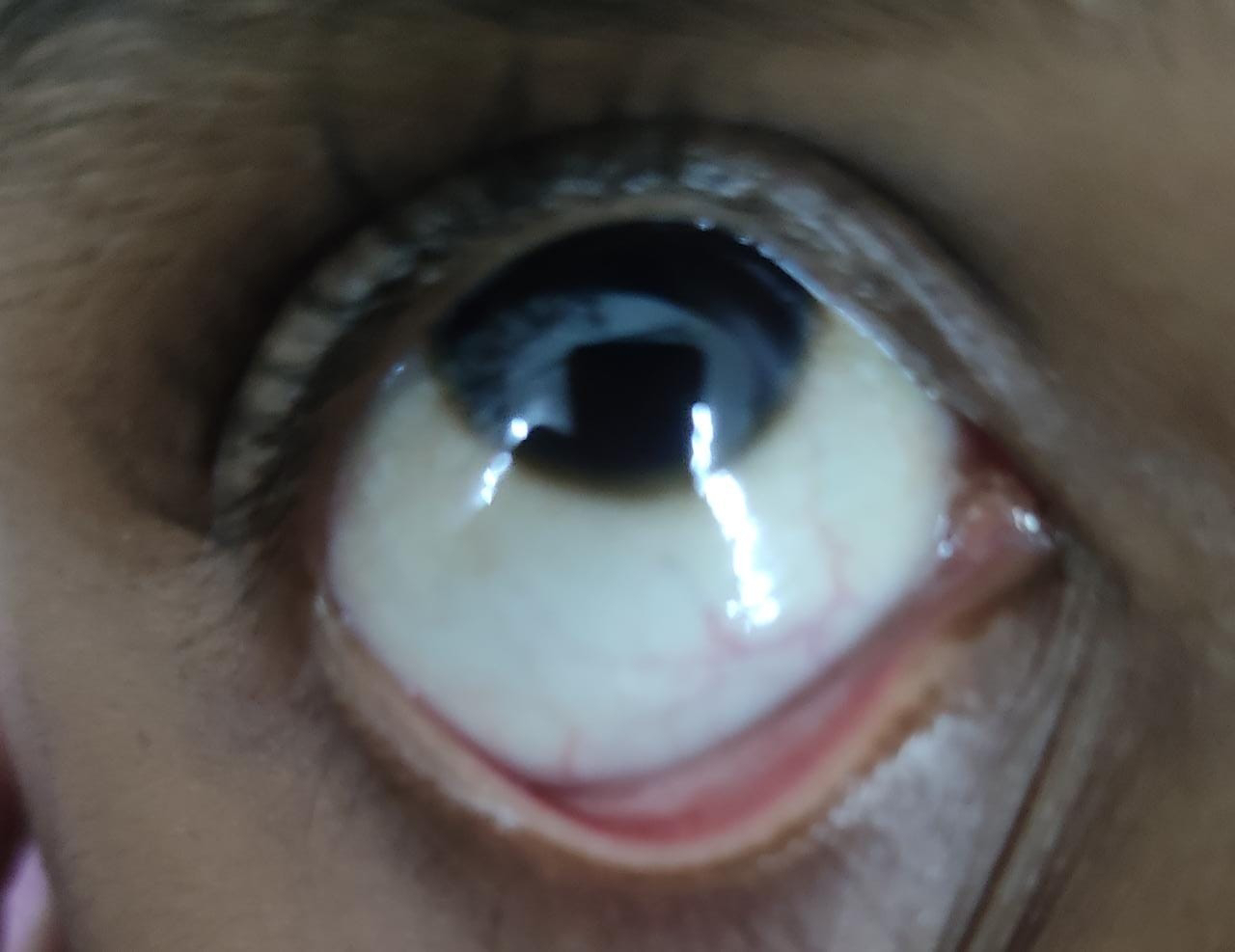
We took ophthalmology opinion
but on examination, in both the eyes NO changes of diabetic retinopathy noted.
















Comments
Post a Comment