A 70 years old building constructor with altered sensorium and cough.
This is an E log book to discuss our patient's de-identified health data shared after taking his guardian's signed informed consent. Here we discuss our individual patient problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable comments in comment box are most welcomed
I have been given this case to solve in an attempt to understand the topic of "Patient clinical data analysis" to develop my competency I reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
A 70 year old male building constructor by occupation presented with chief complaints of
Cough and SOB since 20 days
Altered sensorium and
Fever since 3 days
Burning sensation in the oral cavity since 2 days
#History of present illness #
Patient was apparently asymptomatic 20 days back when he developed cough followed by alcohol binge which was associated with sputum.It was of small quantity,non foul-smelling, non blood tinged.
He also complained of shortness of breath which progressed from grade 2 to grade 4.(NYHA)
Fever since 3 days ,dissolved by medication.
He also complained of burning sensation in the oral cavity and was unable to take food and talk.Initially he developed throat pain later he noticed some painful vesicles over the soft palate.
He was taken to government hospital and he was treated symptomatically over there.But his sensorium was deteriorating so he was referred to our hospital.
On the day of presentation, patient was in altered sensorium state,tachypnic,drowsy,but arousable
There is no history of orthopnea,paroxysmal
nocturnal dyspnea.,palpitations and sweating.
#past history #
H/o exposure to dust for long hours due to his occupation for 30-35 years
No h/o htn,dm,epilepsy, asthma,TB,CAD
#personal history #
Mixed appetite
Adequate sleep
Bowel and bladder movements regular
Addictions: Alcoholic since 30 years
H/o tobacco usage in the past.
No known allergies
Family history
No history of similar illnesses among immediate family members.
No significant family history.
The patient lost his first wife to an unknown illness 30 years ago. He has 2 daughters with his second wife.
General examination
Patient was examined after taking an informed consent. Patient is conscious coherent cooperative and well oriented to time, place and person.
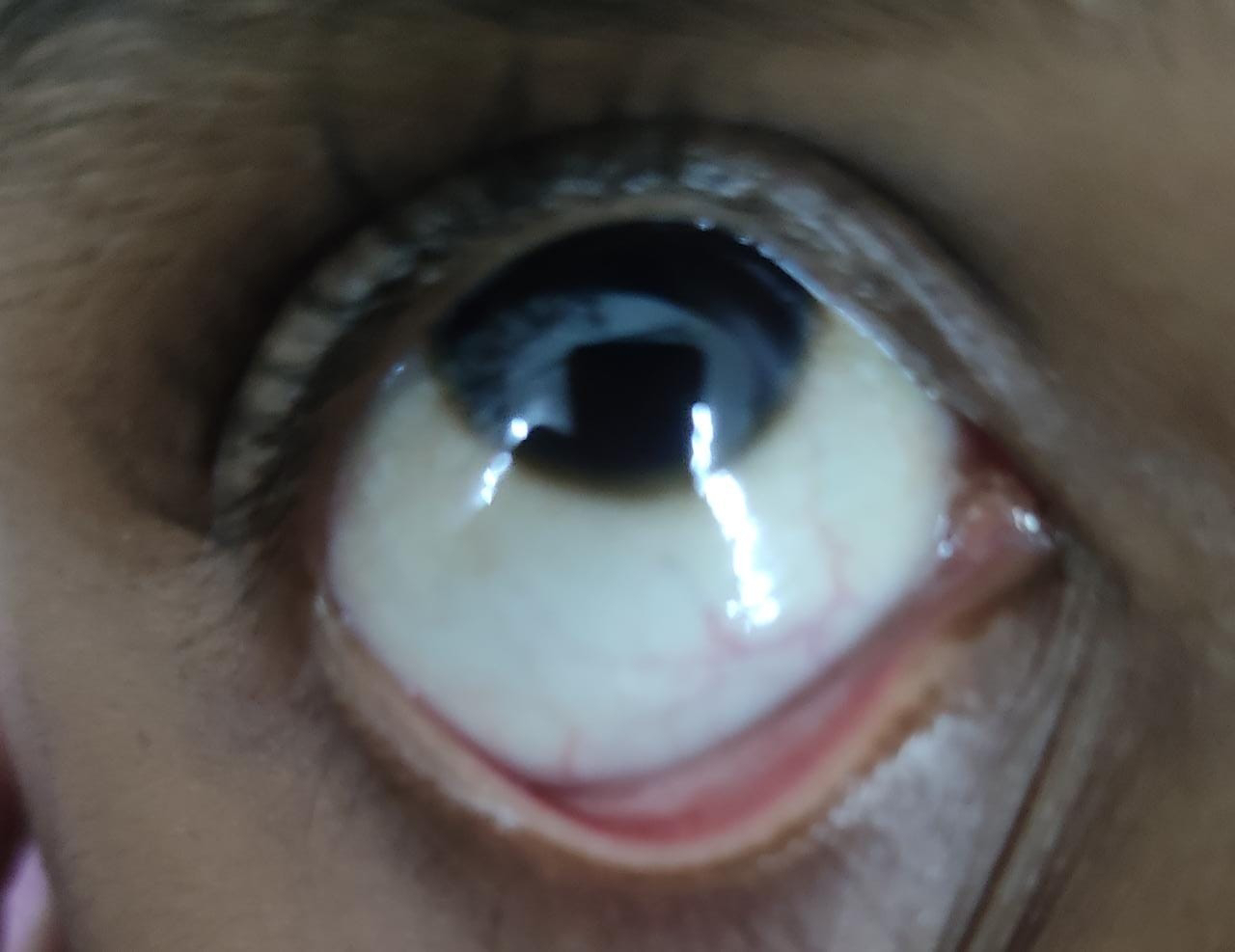
No sign of pallor,icterus ,clubbing, lymphadenopathy,generalised edema.
VITALS:
PR: 87 bpm
BP: 120/70 mmHg
RR: 18 cpm
SpO2: 98%
Temperature: afebrile
Systemic examination
Respiratory system: oo 13.1.2022
inspection:shape of chest elliptical
No drooping of shoulder
Supraclavicular hollowness present
No visible sinus,scar or crowding of ribs
trachea central in position.
Palpation: inspectory findings are confirmed
No tenderness or local rise of temperature
Percussion: no dull note
On auscultation:bilateral air entry present
No Creptititions or any added sound present
CVS: S1, S2 heard, no murmurs
Abdominal examination:
Inspection:
Shape of abdomen -scaphoid
Position of Umbilicus- Central and inverted
All Quadrants of abdomen moving with respiration.
No visible scars and sinuses.
Hernial orifices free
No visible pulsations.
Palpation :
Soft
No tenderness
LIVER - Not Palpable
SPLEEN- Not Palpable
Percussion :
NO SHIFTING DULLNESS
NO FLUID THRILL
Bowel sounds heard.
CNS:
GCS: E4V4M6
Cranial nerve examination intact
Speech slurred
Sensory system- sensitive to pain, touch , vibration and temperature.
Motor system Right. Left
Power- UL 5/5 5/5
LL 5/5 5/5
Neck ,trunk power normal
Tone- UL Normal Normal
LL Normal Normal
Reflexes-
Superficial reflexes - Intact
Plantar flexion flexion
Deep tendon reflexes -
Biceps ++ ++
Triceps ++ ++
Supinator ++ ++
Knee ++ ++
Ankle ++ ++
Gait- Normal
Cerebellar system - intact
Investigations findings on 7.1.2022
CBP : total leucocyte count 13000 cells/cumm
APTT test : 57 second
CUE : albumin +
Prothrombin time : 28 seconds
FBS : 227 mg /dl
Blood urea: 359mg/dl
ABG : po2 198mmhg
Pco2 19.9 mmhg
Serum Creatinine 5.5 mg/dl
Uric acid 20.3 mg%
Sodium 161 mEq/L
Potassium 7.3 mEq/L
Chloride 117 mEq/L
Us Abdomen for kidney size and architecture of liver
Findins on 8.1.2022
Prothrombin time 26 secs pro(longed
INR prolonged
HEMOGRAM
Impression on smear
RBC: NORMOCYTIC NORMOCHROMIC
WBC within normal limits
Platelets Adequate in number and distribution
No hemiparasites
No monocytes
RFT urea 166
Creatinine 3.8
Uric acid 8.6
Phosphorus 6.9
Sodium 147
Potassium 4.5
Calcium, Chloride Potassium within normal range
Bacterial culture
No growth after 24 hours of incubation
On 10.1.2022
Urea 127 mg/dl
Creatinine 4.5 mg/dl
Sodium 143 mEq/L
Potassium 4.5 mEq/L
Chloride 104 mEq/L
Treatment
Head end elevation
O2 inhalation
Iv fluids NS RL DNS
Inj Lasix 40 mg iv/BD
Inj Piptaz 2.25gn Iv/TID
Inj Thiamine 1Amp in 100 ml NSIv/TI D
Tab Montec- Lc peroral/od
Tab Pulmoclear po /od
Tab Ambroxyl 15ml Po / TID
Mucopain Gel LA BD
Betadine gargle
Bp/PR/ RR/ temperature 4th hely
GRBS 6th hourly
Tab Azithromycin 500 mg Po /DO OD
Nebulisation with Broad spectrum anbiotics
4 sessions of hemodialysis done.
After 1st dialysis he didn't improve. After 2nd dialysis he started taking and after 3rd dialysis he started as asking food.
Provisional diagnosis:
altered sensorium secondary to uraemic encephalopathy, viral pneumonia with acute kidney injury secondary to sepsis.
Improvement


















Comments
Post a Comment